Stretching can be frustrating at first. These practical tips and demonstrations will help you make progress, even if you're super stiff.
Best GMB Articles & Tutorials
🥇 Most Popular Articles & Guides
100s of Free Training Resources
Since 2010, we’ve been sharing articles and videos covering everything you need to know about building physical autonomy – specific skills, training concepts, lifestyle advice, and anything else you could need to feel strong and confident in using your body every single day.
There’s a lot here. Almost too much. So, we put this page together to help you find our most important free resources.
Start here, and don’t worry! There’s plenty of time for us to get to know each other, so take it slow 🙂
🆕 Freshest Updates
🏆 Top Videos
💪 Training with GMB
👏 Client Case Studies
👉 See more GMB client results & reviews
🆓 Learn the Key Movement Patterns Most Workouts Neglect
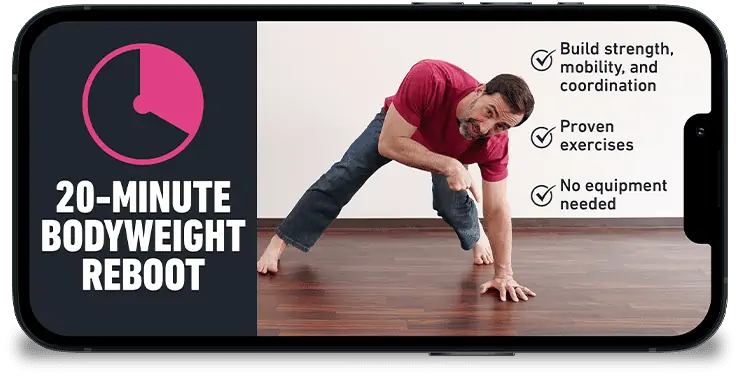
Get the free routine to start building strength and agility right away.
Give us your email address so we can relentlessly spam you with free videos and articles to help you move better without all the aches and pains.