A lot of us grew up hearing that joint pain is the price of an active life.
Running, jumping, squatting, playing — all supposedly wear down the cartilage until one day you get to “bone-on-bone.” And then, that’s it. Game over!
It’s a simple story that seems like common sense, but it’s also completely wrong.
Modern research shows that osteoarthritis isn’t caused by using your joints, it’s caused by your body losing the ability to adapt to use.
Your joints aren’t car parts that wear out.
Unlike plastic and metal, our bodies are living systems that change in response to the signals we send them, and the most powerful signal of all is movement.
Podcast: Osteoarthritis Discussion with Dr. Howard Luks
 This article was partly inspired by my chat with Dr. Howard Luks for the GMB Podcast.
This article was partly inspired by my chat with Dr. Howard Luks for the GMB Podcast.
Listen while we break down the myths about osteoarthritis and talk about the real connection between movement, metabolism, and joint health.
What’s Really Going On With Osteoarthritis
Osteoarthritis (OA) is often called a “degenerative disease,” but that word creates the wrong impression. It can make us think it’s something that will inevitably leave us in pain as we age.
It’s true that with time we may develop thinning cartilage, bone spurs, and other changes. But these are natural and normal changes; just as we get wrinkles on the outside of our skin, we get wrinkles inside our bodies as well.
Cartilage and other tissues don’t simply wear away like the tread on a tire. They’re constantly remodeling themselves in response to stress.
And yes, we need stress!
Good stress, the kind that comes from appropriate movement and exercise, is what keeps that adaptive process going. When you move, you stimulate the cells that maintain cartilage and lubricate your joints.
When you stop moving, those signals fade, and the tissues become weaker and less resilient.
“Our bodies were engineered to move. We weren’t engineered to sit. If we’re not active, we’re deteriorating.” — Dr. Howard Luks
And unlike the outdated thinking that some doctors still subscribe to, modern medical consensus backs this up. A 2017 statement from the Osteoarthritis Research Society International (OARSI) concluded that exercise (including strength, aerobic, and neuromuscular training) should be considered a core treatment for osteoarthritis in all populations.
In plain terms: movement should be the first choice to make our lives better.
The Real Culprits Behind Osteoarthritis
Chronic inflammation
While movement is protective, chronic inflammation can work against it.
High blood sugar, poor sleep, and low activity all contribute to low-level inflammation that affects every tissue in the body, including cartilage and tendons. It’s why people with metabolic syndrome are at higher risk of developing joint problems, even (and especially) if they’re not particularly active.
Movement helps here too. Strength training, walking, and skill-based practice improve metabolic function and reduce inflammation.
The Johns Hopkins Arthritis Center describes exercise as “the most effective non-drug treatment for arthritis,” improving pain, function, and long-term joint health — even for people with significant osteoarthritis.
No supplement, injection, or procedure can match the long-term benefit of simply getting your body to do what it was built to do.
The MRI problem
A big reason people feel helpless about osteoarthritis is imaging. Once you’ve seen an MRI report that says “degeneration” or “tear,” it’s hard to forget it. It’s easy to worry that you’ll never feel better — or that things will only get worse.
Fortunately, structure doesn’t always match symptoms.
Plenty of people have degenerative changes and feel great. Others have pain with perfectly normal scans.
That mismatch can be confusing and frustrating, but it can also be freeing. It means you’re not doomed by your imaging. You’re not fragile.
“We don’t need to be structurally perfect to function perfectly well.” — Dr. Luks
A large percentage of adults show cartilage or bony changes on imaging of the shoulders, hips, knees, and spine — yet most have no pain at all. Hip tears | Hip FAI | Meniscus tears| Shoulder tears | Spinal degeneration
This is not to say that if you have these changes, that your pain isn’t real.
Absolutely not.
It’s to remind you that pain is complex, and there are many reasons your knees or hips might be bothering you. More importantly, there are many ways to get better.
Why Rest Can Make Osteoarthritis Worse
When your knee or hip hurts, resting feels like the smart move. But rest won’t fix OA — and too much inactivity can actually make you feel worse.
Without movement, tissues weaken and stiffen. The nervous system becomes more sensitive to pain signals. You end up feeling more fragile, not less.
Instead, practice intelligent loading — moving within a range that challenges your body just enough to rebuild trust and capacity.
“We have to acknowledge the pain, we have to acknowledge that it exists, adjust how we’re going to load accordingly. But we have to make it clear that we can’t avoid discomfort during the process. And that’s part of the healing, and that not all pain implies harm.” says Luks.
That’s consistent with the evidence: the Johns Hopkins Arthritis Center highlights that strengthening and range-of-motion exercises improve comfort and stability far more effectively than inactivity.
The right kind of challenge is what keeps your joints healthy.
Osteoarthritis Q&A — Movement & Exercise Questions
Can I still exercise if my doctor told me I won't be able to run or jump again?
Exercise helps your body adapt, strengthens the muscles that support your joints, and stimulates the tissue repair processes that keep cartilage healthy.
The key is to train within a range that challenges you and to stay consistent. Inactivity, not movement, is what accelerates decline.
What if my joints are bone-on-bone, can I still exercise?
It’s normal to feel some discomfort when you begin moving again, but pain doesn’t always mean harm. The right kind of stress teaches your body how to tolerate load again.
How can I exercise without aggravating my osteoarthritis?
A simple rule of thumb: aim to keep discomfort during exercise at 3 out of 10 or less on your personal pain scale. You should feel some effort or mild achiness, but not sharp pain or anything that lingers or worsens afterward.
When starting (or restarting) activity, begin with about 50% of what you’d normally do, then slowly increase over time. This gives your joints and tissues room to adapt.
Also remember that flare-ups aren’t always immediate — sometimes irritation shows up a few hours later or the next day. Starting with less helps you learn your body’s response and build confidence as you go.
Consistency and gradual progression matter far more than intensity. The goal isn’t to avoid all discomfort, but to teach your body it can move safely again.
Can osteoarthritis be prevented?
But you can absolutely influence how your joints age and how well they function.
Regular movement, strength training, and skill-based exercise help your joints stay adaptable and resilient. They keep cartilage nourished, muscles strong, and your nervous system confident in movement.
Good sleep, balanced nutrition, and maintaining metabolic health also reduce the chronic inflammation that can accelerate joint changes.
Think of it less as “preventing” a disease and more as building joint resilience. You may still develop some structural changes over time, everyone does, but those changes don’t have to mean pain or loss of capability.
The real goal isn’t to avoid change, it’s to have the ability to adapt well.
The Three Attributes That Keep Your Joints Healthy And Strong
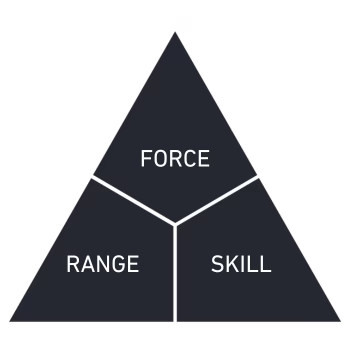 At GMB, we describe physical capability through three primary attributes: Force, Range, and Skill.
At GMB, we describe physical capability through three primary attributes: Force, Range, and Skill.
Together, they’re the framework that helps your joints keep up with everything you want and need to do.
 1. Force: Improved Strength Capacity Builds Shock Absorption
1. Force: Improved Strength Capacity Builds Shock Absorption
Strong muscles act as shock absorbers, reducing strain on your joints. They also offer benefits beyond that.
“Our muscles are an internal pharmacy,” said Luks. “They release hundreds of beneficial chemicals when activated.”
This is part of the metabolic process – properly stimulating your muscles produces substances that counteract inflammation and support recovery.
 2. Range: Improved Mobility Builds Room For Error
2. Range: Improved Mobility Builds Room For Error
Good range of motion through your limbs and spine is also essential for joint health.
Stiffness means repetitive forces hammer the same areas again and again. While your body can adapt, there’s a point where too much stress outpaces recovery.
That’s what we mean by appropriate loading in exercise, balancing enough stimulus to grow stronger without tipping into overload. Better mobility gives you more margin for error, allowing forces to distribute instead of concentrate.
 3. Motor Control: Improved Control Builds Physical Capability
3. Motor Control: Improved Control Builds Physical Capability
This one’s less intuitive but just as critical.
Strong muscles are great, but you also need to know how to use them well. A 2022 paper in Frontiers in Medicine found that improving balance, coordination, and proprioception alongside strength training reduced pain and improved stability more than strength work alone.
“Yes, we decline with aging, but we decline far greater than what aging has in store for us simply because we don’t train it anymore,” says Luks. “At 63 I still rock climb, run, and do your Bear and Monkey movements. I’m not as mobile as your instructors, but I’m doing it.”
When Surgery or Other Treatments Make Sense for Osteoarthritis
Most joint and tendon problems get better with time, consistent rehab, and the right kind of loading. But sometimes, even with the best conservative approach, pain and dysfunction persist.
That’s when other options such as targeted procedures and surgery can help.
The key is context. Imaging alone doesn’t decide it; your function and quality of life do.
“I’m not the one who determines when you need an operation — you are,” says Luks.
When you’ve given exercise, therapy, and patience an honest effort, and your pain still limits what you can do, that’s when the surgical conversation starts to make sense.
Certain structural problems don’t respond to rest or exercise alone. Some meniscus tears, like “root” or “bucket handle” types can cause locking or severe pain and may threaten the joint’s long-term health. Occasionally, a small loose flap in the knee that refuses to calm down after months of rehab might need a cleanup.
 For younger, active people with poor alignment and knee arthritis on only one side of the knee, a high tibial osteotomy (realigning the leg to distribute forces better) can preserve activity when a total replacement would be too restrictive.
For younger, active people with poor alignment and knee arthritis on only one side of the knee, a high tibial osteotomy (realigning the leg to distribute forces better) can preserve activity when a total replacement would be too restrictive.
There are other treatments that can support healing.
Shockwave therapy can possibly jump start recovery in stubborn tendons, PRP injections may help if they are high quality and given to the right conditions, and Tenex can clear out degenerated tissue in select cases. And the old standby cortisone still has a role for short-term relief, though repeated use can be an issue.
Whatever path you choose, remember these interventions work best when paired with smart, progressive loading. They can open the door, but movement practice gets you walking through it.
These kinds of interventions can make a big difference when used thoughtfully, but they’re still tools, not the singular thing you should do. And as options like PRP, peptides, and other biologics continue to evolve, it’s worth understanding what the science actually supports and how these treatments fit alongside the foundation of good movement.
If you remember only one thing here, it’s that many treatments can support the process but they are best used in combination with your tissues being exposed to the right kind of training afterward.
Exercise is an essential part that makes the intervention work.
What gets you back into what you love doing is teaching your body how to trust movement again
Osteoarthritis Q&A — Lifestyle & Treatment Questions
When should I consider surgery?
Procedures like repairing specific meniscus tears, realigning the knee with a high tibial osteotomy, or joint replacement can restore quality of life when conservative care fails.
It’s a shared decision based on your goals and overall function, not simply an MRI report.
What about injections, PRP, or other biologic treatments?
Results depend heavily on the technique and follow-up rehab. These treatments can help tissues recover faster, but the real progress comes from rebuilding strength and coordination through exercise.
Does my bodyweight affect osteoarthritis?
But it’s also a bit of a “chicken and egg” situation.
If someone is dealing with **metabolic syndrome** (combination of high blood pressure, high blood sugar, elevated cholesterol, triglycerides, and/or increased abdominal fat) the resulting chronic inflammation can make joints more painful and less resilient.
As you move better and support your overall health, inflammation drops, your joints function more efficiently, and pain often decreases, regardless of what the scale says.
Can diet and nutrition help with osteoarthritis?
Focus on nutrient-dense foods — lean proteins, colorful vegetables, fruits, and healthy fats. Limiting processed foods, excess sugar, and alcohol helps reduce systemic inflammation.
You don’t need a perfect diet; you need one that’s balanced, consistent, and supports your activity level. A healthy metabolism amplifies the benefits of movement.
You’re Not Falling Apart: The Real Cause of Decline Isn’t Aging
We don’t lose capacity because we get old, we get old because we lose capacity, and most decline comes from disuse, not age.
Strength, balance, and coordination fade only if you stop training them, and they come back as soon as you start.
What You Can Do Right Now
- Move daily — even small amounts.
- Train strength with control.
- Prioritize sleep and good nutrition.
- Don’t panic about scans.
- Stay curious and patient.
Build your resilience and capacity, these will serve you much better than quick fixes.
Training Your Body to Move Better
Osteoarthritis shouldn’t be seen as punishment for a life well lived. Nor is it a stop sign that prevents you from continuing to do what you love.
You just have to adapt wisely and give your body good inputs; more movement, proper loading, and better control.
Movement is the medicine, and capability is the cure.
Start with Elements
The best way to rebuild trust in your body is through simple, consistent practice. Elements gives you the foundation: strength, mobility, and control, all in one approachable program. Start where you are, and build capability that lasts as long as you do.





